By Dr. Richard Schoske, Chief, Diagnostics & Detection Division (CBA), Chemical & Biological Technologies Department (CB), Research & Development Directorate (RD), Defense Threat Reduction Agency (DTRA) and Mr. Michael Boeri, DTRA RD-CBA, Fort Belvoir VA, USA
“Re-imagining biothreat detection”
The threat faced from infectious biological agents continues to increase at a substantial rate. This is attributable to a number of factors including increased globalization, climate change, and the emergence of novel biotechnologies. The SARS-CoV-2 pandemic, which has affected the entire global population and brought about numerous unseen challenges throughout society, is clear evidence of the aforementioned threat. The development and large-scale implementation of both laboratory and at-home tests was likely beneficial in mitigating the spread of disease. However, this new reality was not matched with new solutions. These testing platforms have been in use for decades and their shortcomings were exposed in the form of their slow rollout (antigen tests) and requirement for laboratory processing (PCR). In order to better manage future biological threats, it is essential to explore and pursue diagnostic technologies that go beyond the traditional paradigms.
These paradigms are routed in pathogen-directed identification which often involve invasive collection techniques. Our goal is to develop agnostic approaches that can show a positive result before symptom onset, regardless of the pathogen that is present in the sample. These approaches also aim to predict severity of disease and thus enable medical personnel to appropriately triage persons afflicted with a pathogen. Finally, these approaches will move away from reliance on intrusive collection methods such as nasopharyngeal swabs or venipuncture.

“Pre-Symptomatic Diagnosis”
Effective management and mitigation of future epi- and pandemics will rely on a technology that goes beyond what currently exists in the field of biodetection, which until now is prompted only when a patient feels ill or believes they may have been exposed to someone who is infected. As has been seen in the past three years, existing testing technologies simply are not able to keep up with a highly-transmissible infectious agent, and in most cases, testing is done too late to effectively prevent a subject from exposing and/or infecting others.
A concept that is being active and aggressively pursued is pre-symptomatic diagnostics. In general, the process of contracting a biological agent takes place in four general steps: exposure, assimilation, infection, and disease. By the time a sick individual takes a test, they will likely have reached the disease stage of illness, which manifests itself in the traditional symptoms that typically lead a person to believe they are ill; however, prior to progressing to the disease stage, there are atypical biochemical processes occurring in the host that are only initiated during the assimilation and infection phases. The goal of this effort is to identify these host-based biomarkers that are expressed during the pre-symptomatic window and develop assays that are both sensitive and selective enough to be implemented in a new testing device.
A core facet of these projects is to understand which of these biomarkers are upregulated and expressed as a function of different bacterial and viral infectious agents. There is strong evidence that several of these biomarkers are threat-agnostic, as in they are upregulated in the host following infection with several different biological agents (e.g. bacterial vs. viral). By utilizing this approach and leveraging these threat-agnostic biomarkers, testing could be done in a way that informs the patient not specifically what they are infected with, just that they are infected with “something”. Patients testing positive on such a test would then follow up with the traditional genomic testing to confirm the identity of the infectious agent and seek the appropriate treatment.
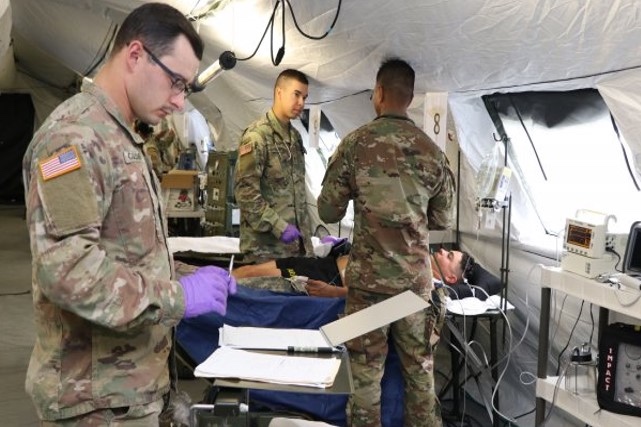
The host-based biomarker paradigm has been integrated into a prototype device that is currently being evaluated by the U.S. Military. At present, the U.S. Navy is conducting trials with one such device in human patients as part of a humanitarian mission underway by one of their hospital ships. This device utilizes a saliva sample from the patient to screen for various host-based biomarkers that were identified during the research and development phases of the product [1]. Results of this study will aid in the continued development of this technology towards the end goal of widespread public implementation.

“Predicting Disease Severity”
A shift toward sampling for host-based biomarkers in biological screening also creates a new opportunity for medical personnel to potentially predict the severity of disease a patient may experience. Efforts are currently underway to expand technology currently being used to improve sepsis care in hospitals towards a new tool that can identify a specific set of biomarkers that accurately predict disease severity for a broad panel of infectious agents [2]. Patterns in both the identity and expression levels of these biomarkers in the body at a given stage of illness are compared to normal physiological baseline conditions, providing medical personnel with a disease progression “forecast”.
The developers of this technology begin by collecting a clinical sample from the patient, measuring a large set of biomarkers in that sample, and comparing the results against a database that has been established using extensive sets of patient samples and assaying a broad range of analytes in those samples. By creating this extensive and diverse historical dataset of biomarkers from these patient samples, advanced machine learning algorithms are capable of parsing the data such that one is now effectively able to rapidly identify individuals at risk of severe disease outcomes. Further efforts are required for this technology to approach the forefront of medical care, but as the power of artificial intelligence and machine learning (AI/ML) tools continues to grow, it is likely that these development efforts will benefit greatly in the months and years to come.
“Minimally-Invasive Sampling”
When it comes to collecting the patient samples needed for these diagnostic tests, current technologies almost universally rely on invasive sample collection techniques such as nasopharyngeal swab, saliva sampling, and venipuncture. In an effort to expand these diagnostic sample matrices and ease the burden of sample collection, several studies are currently underway exploring the feasibility of using exhaled breath as a novel, non-invasive testing method. While several breath sampling tests have been approved and employed the past (e.g., tuberculosis and COVID-19 breath tests [3]), they have proven neither accurate nor robust enough to fully replace the current testing protocols.
The efforts currently underway are focused on establishing a baseline profile of the constituents of normal, healthy human breath and building an understanding of the metabolic pathways that generate these breath features. Specifically, these studies will capture volatile organic compounds (VOCs) and non-volatile exhaled breath components (EBCs) from a population of healthy individuals and identify volatile metabolites, proteins, and lipids from these samples. Statistical analysis will then be performed to determine the profile of features conserved in a defined fraction of the population and those features will be mapped to metabolic pathways to elucidate the biological source of breath features. Lastly, an algorithm will be developed using ML to identify breath signatures, which will enable the development of a future diagnostic platform using breath as a sample matrix.

The Department of Defense is currently funding such an effort, which aims to deliver a compact, handheld device that captures the VOCs from a patient’s breath to provide an early diagnosis of both bacterial and viral respiratory infections. This capability will allow for early implementation of countermeasures such as isolation, quarantine, and removal from an area, potentially reducing transmission, morbidity, and mortality rates. In addition, implementation of breath sampling will likely lead to increased testing compliance among the population due to its ease and lack of invasiveness to the patient.
“Closing Statement”
As we continue to witness the emergence of new infectious diseases, it is critical to re-imagine the way we approach the processes and protocols for identifying and assessing the effects of these pathogens on the population. As biological threats rapidly evolve, novel agnostic approaches are required to account for the threat they pose to the population. Thus, we are making a concerted effort to transition our efforts towards novel, host-based diagnostic approaches. Based on these threats, we feel that pre-symptomatic diagnostic approaches, the ability to predict disease severity, and the pursuit of minimally invasive sample collection techniques all have significant potential to help re-imagine testing and alleviate and/or minimize the impact posed by emerging biological agents.
About the Authors:
Richard Schoske, PhD, serves as Chief of Diagnostics and Detection Division (RD-CBA) for the Defense Threat Reduction Agency (DTRA). In this capacity Dr. Schoske oversees and manages an extensive Research and Development Portfolio that includes projects in the areas of medical diagnostics and chemical and biological agent detection. He has applied this knowledge in operational work experiences involving the development and deployment of novel medical diagnostic systems for the United States Air Force. Dr. Schoske has an extensive background in counter Chemical-Biological Consequence Management Planning. Prior to joining the DTRA, Dr. Schoske served in the United States Air Force for 21 years and is a retired Lieutenant Colonel. During his time on active duty, he served in numerous capacities including Chief of a Medical Laboratory, Assistant Professor of Chemistry at the United States Air Force Academy, Principal Investigator in Diagnostic R&D, and Emergency Medical Planning. He was selected as a Senior Air Force Laboratory Fellow for Science and Technology and is an American Society of Clinical Pathologists Certified Medical Technologist. He earned a Master’s of Arts in Biochemistry from the University of Scranton, and a PhD in Chemistry from American University in Washington DC.
Michael Boeri, MS, provides contractor divisional support to DTRA RD-CBA. He worked as a researcher at the United States Army Medical Research Institute for Chemical Defense (USAMRICD) on several projects related to the development of medical countermeasures to treat the effects of exposure to chemical agents. These include the development of a novel, handheld diagnostic platform to inform an individual of exposure to chemical agents. He earned a Master of Science in Biochemistry from the University of Delaware.





