By CDR (MC) PD Dr. med. Alexis Rump MHBA, Cpt (MC) Cornelius Hermann, Maj (MC) Dr. Med. Patrick Ostheim, Maj (MC) Dr. med. Julian Haupt, Maj (MC) Dr. med. Leonard Kaatsch, and Col (MC) Prof. Dr. med. Matthias Port of the Bundeswehr Institute of Radiobiology, Munich Germany
The threat of “dirty bombs”
Besides nuclear bomb detonations, radiation accidents of different scales may happen in nuclear power or recycling plants as well as in other industrial or research facilities handling radioactivity. An underestimated issue is the loss or theft of radioactive material that may be used for the construction of a “dirty bomb”, combining a conventional explosive device with radioactivity. Such a radiological weapon is much easier to construct and to handle than an improvised nuclear device (IND). The radionuclides used for a “dirty bomb” are impossible to predict, but will primarily depend on availability. Cesium-137 is certainly of great concern, as cesium chloride is a powder that will spread easily. Further critical materials include plutonium or americium. The latter is for example included in smoke alarm devices and so easy to get, at least in small amounts. Despite the facility of construction, a “dirty bomb” attack has never occurred till now. However, there are indications that actual preparations for such an attack have happened several times during the last decades. Thus, a “radiological attack” is a real possibility that must be taken seriously by security forces and a sufficient level of preparedness of emergency services seems mandatory.

Three types of injuries
As with every explosive device, victims in the vicinity of the detonation point will suffer blast injuries: This includes primary blast injuries by the contact of the shock wave with the body and stress and shear forces. In particular the blast lung will lead to respiratory failure in the further course. Victims may also be hit by high velocity primary or secondary fragments with resulting penetration injuries (= secondary blast injuries). By the body being propelled onto surfaces or objects, blunt injuries (= tertiary blast injuries) may be expected as well as burns (quaternary blast injuries). Conventional trauma is suited to cause conditions that are immediately life threatening.
In addition to mechanical trauma, injuries resulting from the specific radioactive additive must be expected (= quinary blast injury). External irradiation by ionizing radiation may occur, and depending on the activity included in the “dirty bomb”, the dose rate of the radiation and the time of exposure, this may induce an acute radiation sickness. However, many hypothetical scenarios that have been studied seem to indicate that such deterministic radiation effects, although they cannot be excluded in individual cases, are not the major threat in the case of a “dirty bomb” attack. In the planning scenarios developed by the Homeland Security Council (HSC), the large scale radiological attack (scenario 11) with a total of 540 fatalities and 810 mechanically injured victims does not include a single case of an acute radiation sickness.
The third type of injuries results from the contamination of people with radioactive dust. Although a large fraction of radioactive material will fall down on the ground at a short distance of the point of detonation, there will most probably be a dispersion of radioactivity on a large surface leading to an external contamination of a large number of people. It must be expected that the number of people radioactively contaminated to different extent will by far exceed the mechanically injured victims. External radioactive contamination is principally associated with the danger of radionuclide incorporation through ingestion, inhalation or through wounds, leading to internal contamination of the body. With exceptions (e.g. the Litwinenko case), the radiological doses caused by radionuclide incorporation are insufficient to cause acute radiation sickness. However, the long lasting irradiation from inside the body is associated with stochastic damages (e.g. mutations) leading to health impairments in the long run. It was shown that on the average a committed effective dose of 1 mSv will reduce the statistical life expectancy by 0.4 days.

Treatment priorities
Self-protection is a basic principle for emergency service members. Externally irradiated patients do not pose a threat to their environment as they are not by themselves a source of radiation. However, victims of a “dirty bomb” attack may be contaminated with radioactive dust. Past experiences indicate that the deposited activity is not expected to cause dose rates that are dangerous to rescue personnel considering the time of exposure. However, rescuers must protect themselves against secondary contamination that may lead to radioactive incorporation. Although heavy NRBC protection suit is certainly adequate, “lighter” equipment permitting an easier handling of the patients is sufficient: This includes wearing protective clothing, respiratory protection (particle filter mask protecting also the eyes) and gloves as used in an operation theater (preferably two pairs) (Figure 1). There is generally no reason for fears approaching the victims and the treatment of the patients must not be delayed by unjustified anxiety about radiation.

Mechanical injury may lead to an immediately life threatening condition (e.g. tension pneumothorax, massive abdominal hemorrhage) and therefore unspecific life saving measures adapted to the acute functional impairment is the first priority. Common traumatology triage systems as well as general principles of emergency medicine (e.g. as Pre Hospital Trauma Life Support System, PHTLS) must be applied in case of mass casualties.
Although probably not a major issue, the possibility of deterministic radiation effects should not be ignored. Development is characterized by the occurrence of prodromal symptoms (e.g. gastrointestinal symptoms as nausea, vomiting and diarrhea, fever, headaches) within hours or days. After an apparent recovery lasting days to weeks (lag time), the symptoms of the acute radiation sickness develop (hematopoietic syndrome with infections, bleedings, at higher doses in addition gastrointestinal syndrome). In order to assess at an early point in time whether a potentially irradiated victim is threatened by an acute radiation sickness and the severity of the expected condition, the time of occurrence of prodromal symptoms in combination with results of blood counts (drop of lymphocytes) permit to state a provisional prognosis. Algorithms based on a data base (SEARCH) gathered from accidentally irradiated patients and implemented in modern software tools permit an easy and fast prediction (e.g. METREPOL, Medical TREatment ProtocOLs for Radiation Accident Victims; H-module as a new scientific triage tool developed at the Bundeswehr Institute of Radiobiology) (Figure 2).
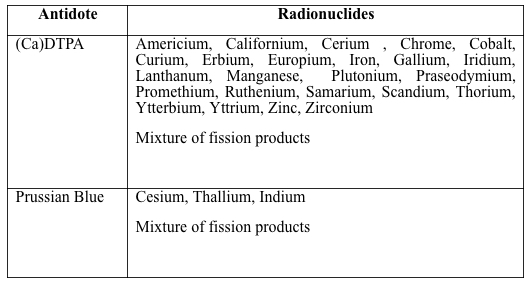
Radionuclide(s) that have been incorporated distribute throughout the body and may accumulate in selective organs where they may stay in part for years and lead to an internal irradiation of the surrounding tissues (e.g. plutonium accumulates in the bone and irradiate the blood forming marrow). The elimination of radionuclide(s) out of the body can be enhanced by decorporation agents, the most important for R&N emergencies being diethylenetriaminepentaacetic acid ((Ca)DTPA and (Zn)DTPA) as well as Prussian Blue (ferric hexacyanoferrate) (Table 1).
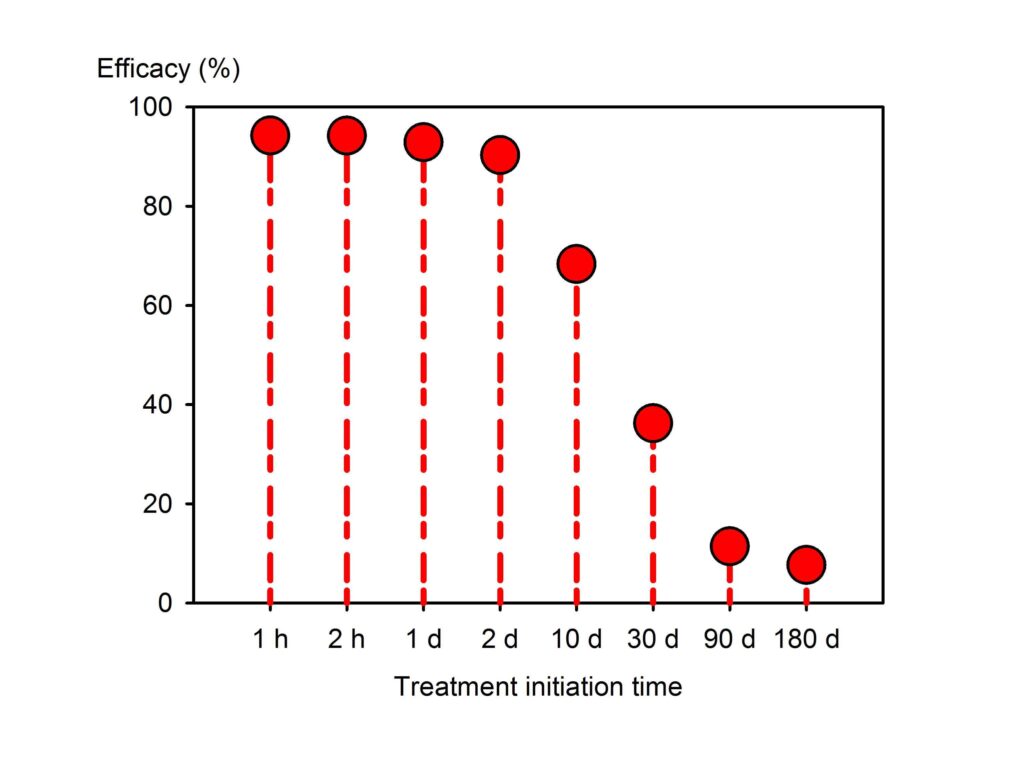
The efficacy of a decorporation treatment is however heavily dependent on the time of therapy initiation as radionuclides sequestered in “deep compartments” (e.g. bone in the case of plutonium) are out of the reach of the antidotes. The loss of efficacy of the treatment over time depends on the radionuclide, the physicochemical properties of the compounds involved and the invasion pathway (inhalation, ingestion or through a wound). Therefore, precise indications on the urgency of treatment initiation cannot be given, but the time slot available for a highly efficacious treatment lies in the range of hours to several days (Figure 3).
The organizational challenges of decorporation treatment
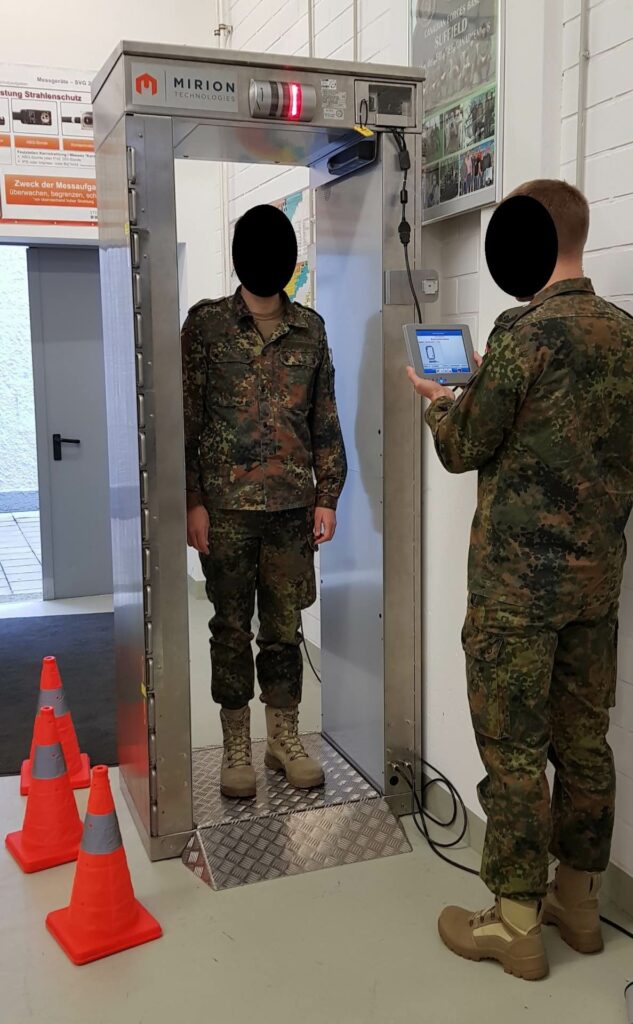
A particular challenge results from the fact that a large number of victims may potentially have incorporated radionuclides. But among them, many victims will not have incorporated substantial amounts of radioactivity and will not actually need decorporation treatment. However, it is not possible to identify patients needing decorporation by simple clinical examination. On the other side, starting decorporation treatment in all victims that potentially could have incorporated radionuclides (“urgent treatment” approach) is associated with huge antidote requirements that for large scale scenarios reach several hundred thousand to several million daily doses, depending on treatment duration. An interesting option to reduce antidote requirements is to use mobile high throughput body counting devices (e.g. monitoring portals) (Figure 4) to identify victims with internal contamination. A further advantage is the positive psychological effect and reassurance of the patient when excluding internal contamination. This may also contribute to relieving the workload at emergency departments of hospitals by avoiding unnecessary visits by worrying patients. It must however be mentioned that the detection limits of such devices heavily depend on the radiation emitted by the nuclide: Whereas it is very useful in the case of cesium-137 that emits gamma rays, it cannot detect radionuclides emitting only alpha particles.
Conclusion
Radiological terrorism is a serious threat although such an attack has never occurred. As radiation accidents are very uncommon, the staffs of emergency services are not familiar with the associated dangers and medical conditions. In many instances there is a particular, emotionally driven fear of everything nuclear and radiological. The basic knowledge required to assess a radiological emergency from a medical perspective is however quite limited. Besides the basics of self-protection, the general rule “treat first what kills first” applies. In addition, a sufficient level of preparedness regarding antidote stockpiling should be ascertained. At the national and international level, specialized institutions may give specific support (as in Germany the Bundeswehr Institute of Radiobiology) to local military or civilian emergency services.
References
1. Rump A, Stricklin D, Lamkowski A, Eder S, Abend M, Port M. Reconsidering current decorporation strategies after incorporation of radionuclides. Health Phys 2016; 111(2): 201-208.
2. Rump A, Stricklin D, Lamkowski A, Eder S, Abend M, Port M. The impact of time on decorporation efficacy after a “dirty bomb” attack studied by simulation. Drug Res 2016; 66: 607-613.
3. Rump A, Stricklin D, Lamkowski A, Eder S, Abend M, Port M. Analysis of the antidote requirements and outcomes of different radionuclide decorporation strategies for a scenario of a “dirty bomb” attack. Am J Disaster Med 2017; 12(4): 227-241.
4. Rump A, Stricklin D, Lamkowski A, Eder S, Abend M, Port M. The incorporation of radionuclides after wounding by a “dirty bomb”: The impact of time for decorporation efficacy and a model for cases of disseminated fragmentation wounds. Adv Wound Care. 2017; 6(1): 1-9.
5. Port M, Abend M. Clinical triage of radiation casualties – The hematological module of the Bundeswehr Institute of Radiobiology. Rad Protect Dosimetry 2018. 182. 10.1093/rpd/ncy141.
6. Rump A, Becker B, Eder S, Lamkowski A, Abend M, Port M. Medical management of victims contaminated with radionuclides after a “dirty bomb” attack. Mil Med Res 2018; 5:27: 1-10 (Open Access: https://doi.org/10.1186/s40779-018-0174-5).
7. Yan T, Lin G, Wang M, Lamkowski A, Port M, Rump A. Pharmacological treatment of inhalation injury after nuclear or radiological incidents: The German and Chinese approach. Mil Med Res 2019; 6:10: 1-10 (Open Access: https://doi.org/10.1186/s40779-019-0200-2)





